Answer of March 2016
For completion of the online quiz, please visit the HKAM iCMECPD website: http://www.icmecpd.hk/
Clinical History:
A 15 year old child with history of acute lymphoblastic leukemia on chemotherapy presenting with acute lower limb weakness.
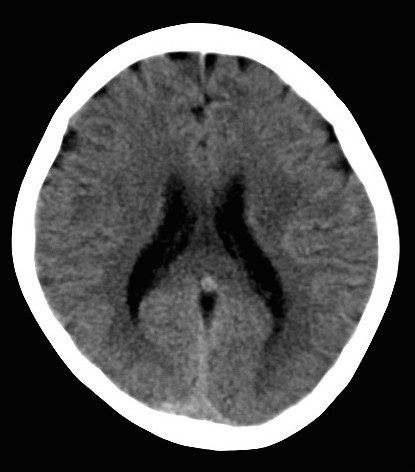
Plain CT Brain
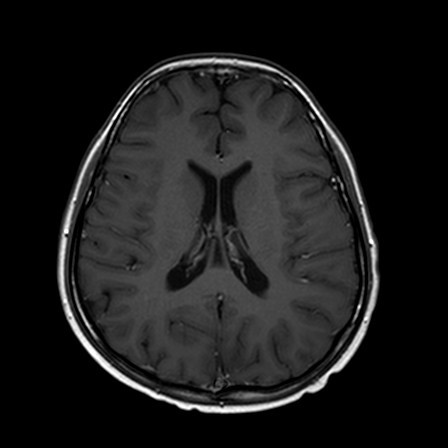
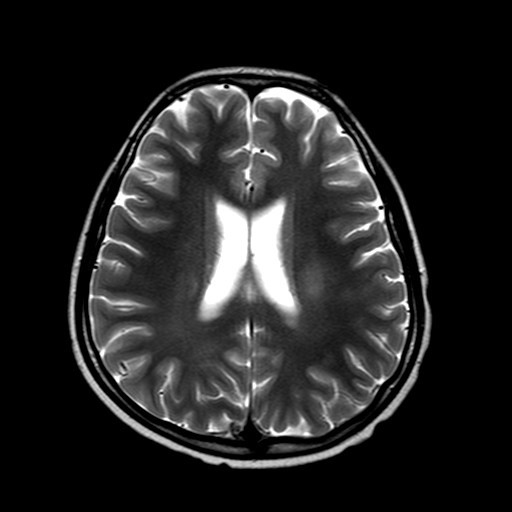
MRI Brain T1W MRI Brain T2W
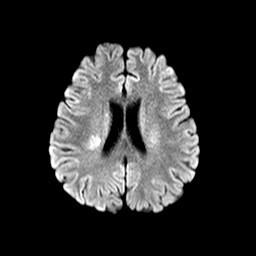
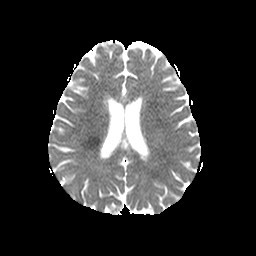
MRI Brain DWI MRI Brain ADC map
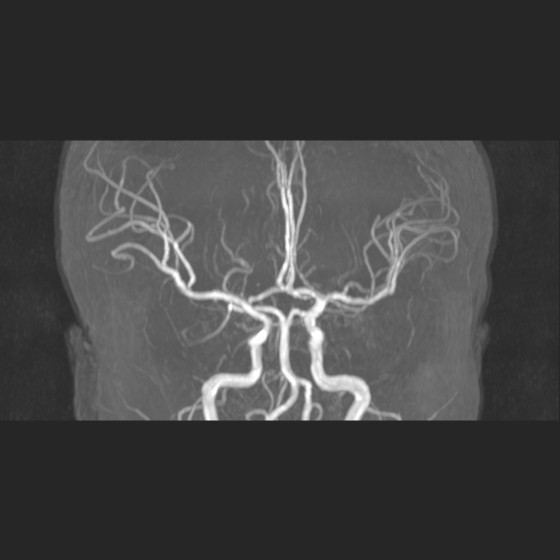
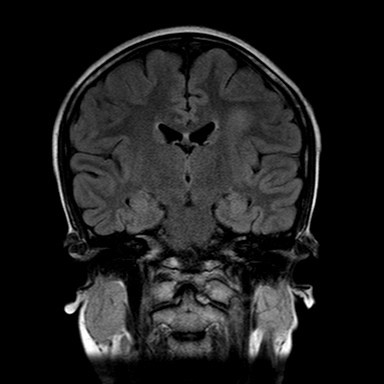
MRA MRI Brain FLAIR
Diagnosis
Methotrexate induced neurotoxicity
Discussion
The incidence of acute CNS neurotoxicity associated with therapy for acute lymphoblastic leukemia is 5-18%. Methotrexate is often the major cause of acute neurotoxicity.
The clinical presentation and the type of neurotoxicity depend on the route and dose of methotrexate. They can present with aseptic meningitis and transverse myelopathy when methotraxate is given intrathecally. Or they can present with acute and chronic encephalopathy as well as stroke-like syndrome with either intravenous and intrathecal methotraxate. Risk facts include high-dose treatment, intrathecal treatment, young age and associated cranial irradiation. In particular stroke-like syndrome usually has onset between 3-10days after administration.
The pathophysiology is unclear. Mechanisms include increased adenosine accumulation, homocysteine elevation and its excitatory effects on the NMDA receptor and alterations of biopterin metabolism.
On MRI, features include T2/FLAIR hyperintensities in the periventricular white matter particularly in the centrum semiovale. Restricted diffusion is present when the disease is detected early. These changes reflect cytotoxic edema.
Patients often recover spontaneously from neurotoxic events.