Answer of January 2016
For completion of the online quiz, please visit the HKAM iCMECPD website: http://www.icmecpd.hk/
Clinical History:
A 13-year-old boy has history of poor vision since 3 years old. Otherwise, no focal neurological sign or abnormal growth was noted. CT and MR of brain were performed to investigate for visual loss.
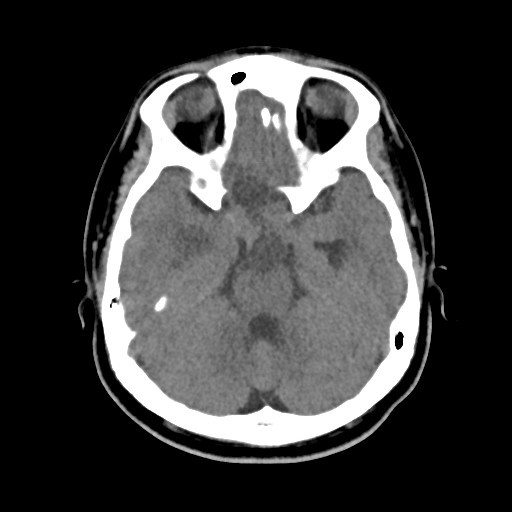
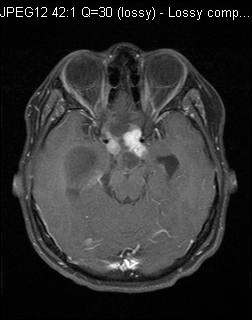
Fig 1. Plain CT Fig 2. MR-T1 weighted axial, with contrast
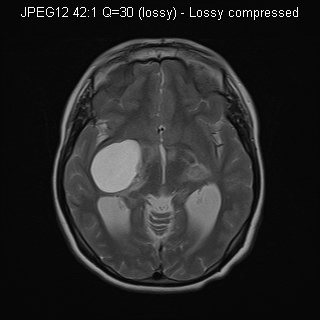
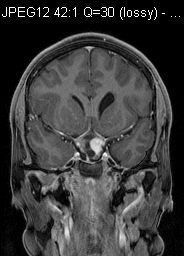
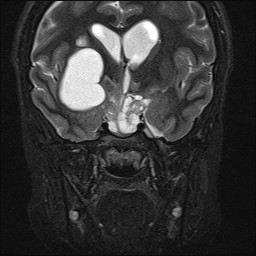
Fig 3. MR-T2 weighted axial Fig 4. MR-T1 weight coronal, with contrast
Fig 5. MR-T2-weighted coronal
Diagnosis
Optic pathway glioma
Discussion
Large suprasellar mass, containing cystic and solid components, are noted, extending to bilateral basal ganglia region. The normal optic chiasm is not identified. Compression of 3rd ventricle is seen, resulting in obstructive hydrocephalus. No intralesional calcification found on the CT. The distribution is along the optic chiasm and optic tract. Imaging features are suggestive of optic pathway glioma. This patient underwent subtotal resection and the pathology shows optic pathway ganglioglioma.
Optic pathway glioma (OPG) is a tumour found predominately in children. It accounts for up to 5% of all childhood brain tumour. Main presenting symptoms are visual disturbance and those related to effect on the optic chiasm and hypothalamus, including precocious puberty, fail to thrive, diabetes insipidus, developmental delay, increased in intracranial pressure, etc. This condition is found in patients with or without neurofibromatosis (NF). In NF group, the most common site of involvement is the optic nerve. In non NF-group, the most common site is optic chiasm and hypothalamus. Non-NF patients tend to have larger tumour at presentation, and the tumours are more mass-like, and frequently with cystic components.
Histologically, OPGs are low-grade gliomas. Majority are of pilocytic type while some are fibrillary astrocytomas. OPG in non-NF patients, however, carry a poorer prognosis, with large proportion of patients showing tumour enlargement even after treatment. Posterior gliomas involving chiasm along optic tract/radiation or hypothalamus tend to carry poorer prognosis as compared to anterior tumour with involvement of optic nerve and chiasm. Other prognostic factors include location, size of the tumour and age of presentation.
Chemotherapy is the initial of treatment for most OPG. Radiotherapy is also potentially efficacious. Surgery may be attempted when the tumour is confined to one optic nerve. Partial debulking, although having no effect on survival, may be used to relieve mass effect and obstructive hydrocephalus.