Answer of August 2015
For completion of the online quiz, please visit the HKAM iCMECPD website: http://www.icmecpd.hk/
Clinical History:
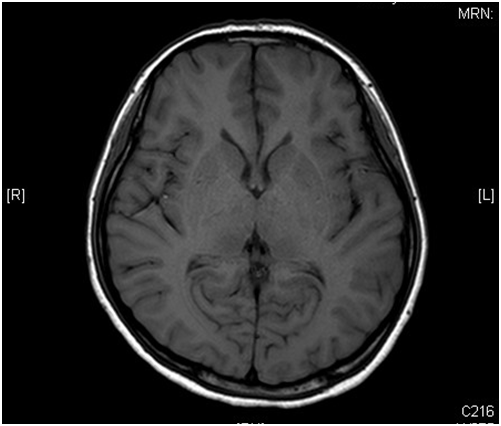
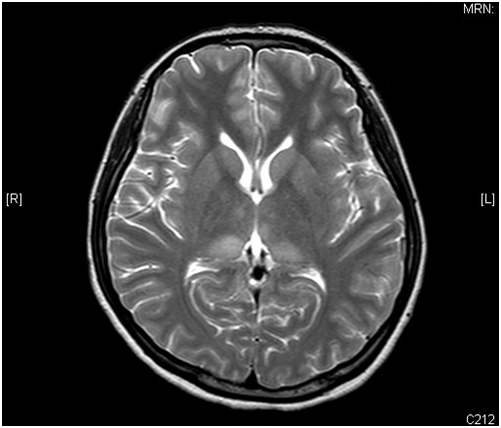
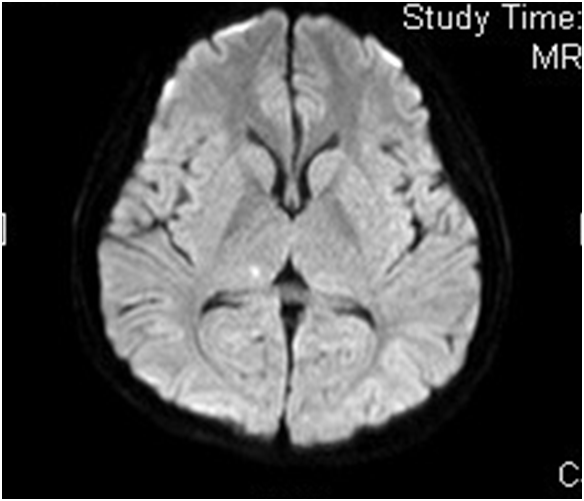
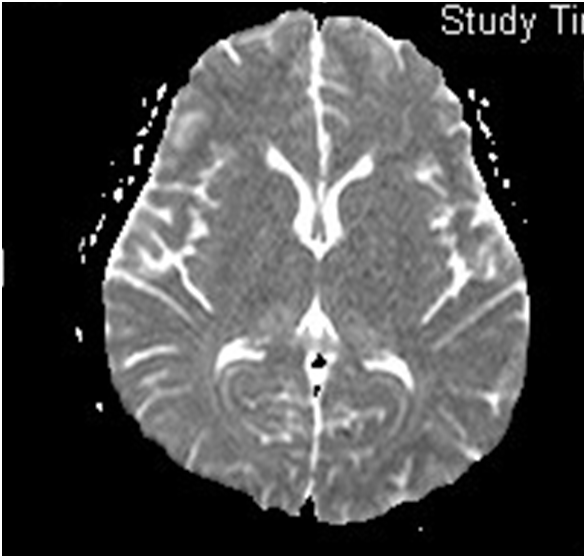
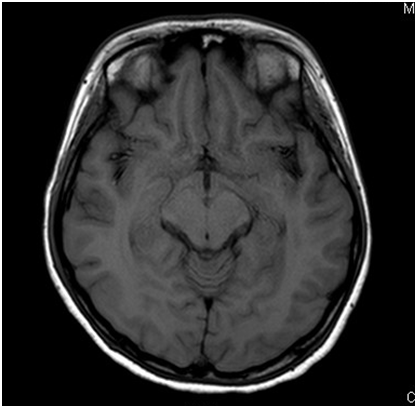
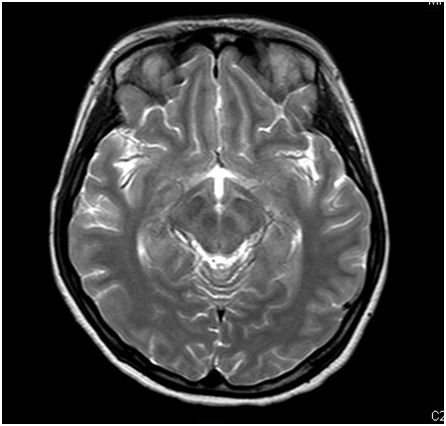
A 21-year old lady presented with fever, headache and confusion for 1 day. Physical examination showed reduced GCS E4V1M5 with neck rigidity. She had history of hiking and mosquito bites. Magnetic resonance imaging (MRI) was performed (6 images – upper row: axial T1-weighted image, axial T2-weighted image; middle row: diffusion-weighted image (DWI), apparent diffusion coefficient (ADC); lower row: axial T1 weighted image; axial T2 weighted image)
DIAGNOSIS
DISCUSSION
Japanese encephalitis is spread by JE virus. It is mosquito-borne by Culex tritaeniorhynchus. It is endemic in Southeast Asia and usually occurs in summer and early autumn. Pigs and birds act as the natural hosts while humans as the incidental hosts.
Majority of the humans infected by this virus is subclinical. The incubation period is about 5 to 15 days. Acute encephalitis can occur in about 2% of all infections, with acute fulminant neurological disease. The mortality rate can be 25%.
In MRI, Japanese encephalitis typically shows bilateral thalamic hyper-intensity in T2-weighted images, unilateral involvement is less common. The basal ganglia, substantia nigra, red nucleus, pons, hippocampus, cerebral cortex and cerebellum can also be involved.
Some lesions, especially those in the thalami, can be hemorrhagic. There is no enhancement in these lesions, indicating only minor blood-brain barrier deficit.
Japanese encephalitis is usually a mono-phasic disease. If the patient survives, he/she would have gradual recovery with or without persistent neurological signs and symptoms. However, biphasic Japanese encephalitis has been described, with early relapse of meningoencephalitic symptoms. In biphasic Japanese encephalitis, the clinical and radiological features can be quite different during the first and second phases.
The differential diagnosis for bilateral abnormalities of the basal ganglia and thalamus are vast, including vascular lesions (e.g. deep venous thrombosis, arterial infarction), CJD, toxic and metabolic lesions (e.g. carbon monoxide poisoning, hypoglycemia/hyperglycemia) or even in neoplastic conditions (e.g. primary lymphoma, glioma, neurofibromatosis type 1).
Correlation of typical imaging features with clinical and laboratory data can help narrowing the differential diagnosis or even make the correct diagnosis.