Answer of March 2007
Clinical History:
A seventy-nine-year-old lady was admitted for percutaneous coronary intervention (PCI). The procedure was uneventful but during the rehabilitation period, she suffered from hypertensive crisis with blood pressure more than 300mmHg. Her urine vanillylmandelic acid (VMA) and cathecholamine were grossly elevated.
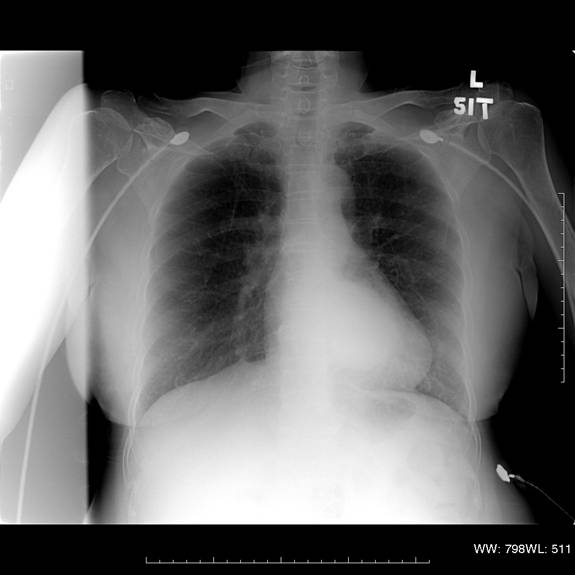
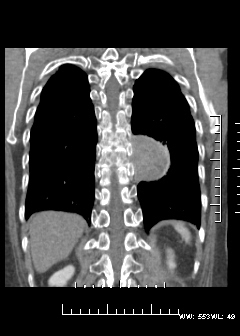
Figure 1
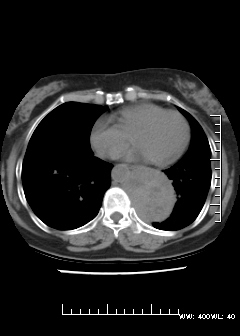
Figure 2
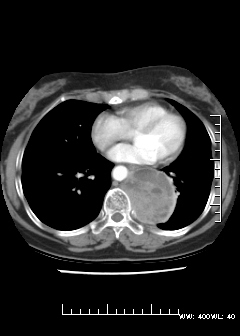
Figure 3
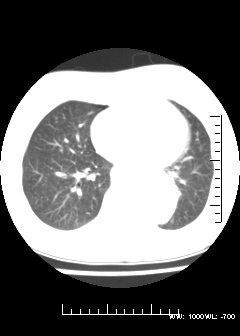
Figure 4: MIBG scintiscan images in 24 and 48 hours respectively
Diagnosis:
Extra-adrenal phaeochromocytoma
Discussion:
When a catecholamine-secreting tumor is suspected, biochemical documentation of cathecholamine and metanephrine hypersecretion should precede any form of imaging study. It is particularly important as this tumor is well known to have varied appearance.
When the lesions are small, they are usually solid but may also present with fatty, cystic and calcified areas particularly in larger lesions. On CT images, most pheochromocytomas have an attenuation of higher than 10HU. Pheochromocytomas typically enhance avidly but can be heterogeneous or show regions of no enhancement due to cystic changes.
Most pheochromocytomas have high signal intensity on T2- weighted MR images because of the high water content, more than 30% have low signal intensity on these images. They are usually hypointense on T1- weighted images but they may be hyperintense if fat and hemorrhage are present. Punctate signal voids representing tumour vessels in paragangliomas create a salt-and-pepper pattern on T1- and T2- weighted images.
123I metaiodobenzylguanidine (MIBG) scintigraphy is often useful when clinically suspected pheochromocytoma cannot be localized. MIBG has almost 100% specificity but limited sensitivity.