Answer of March 2008
Clinical History:
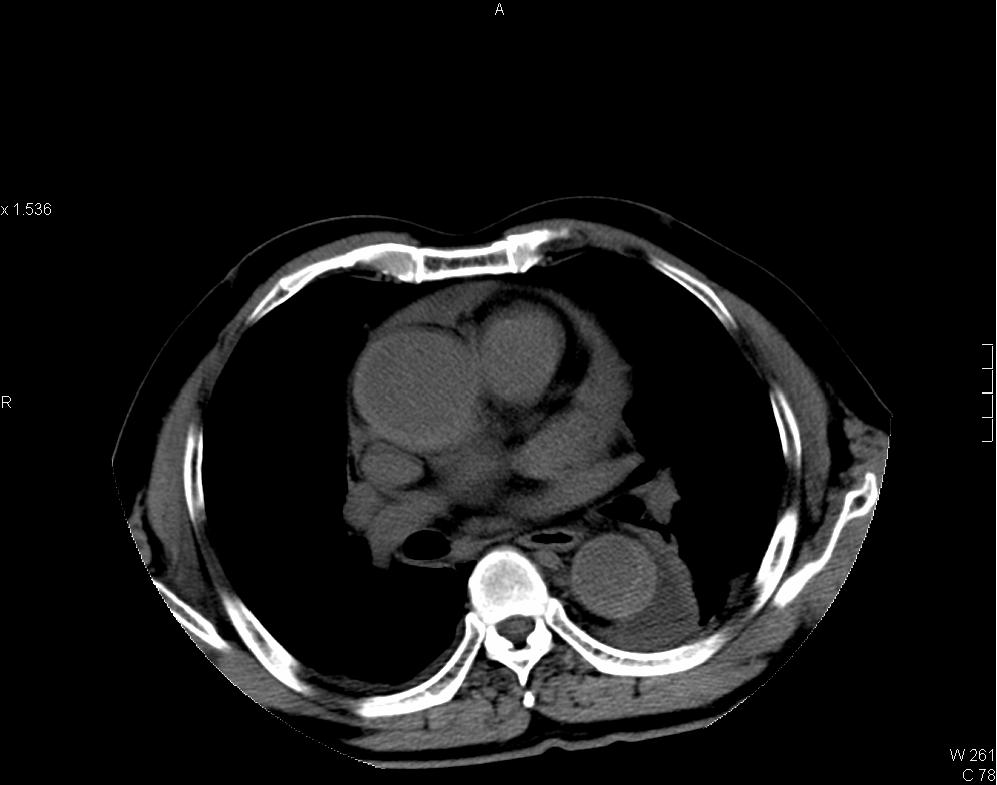
A 73 years old man presented with sudden onset of chest pain. CT thorax performed.
Diagnosis:
Intramural hematoma of thoracic aorta
Discussion:
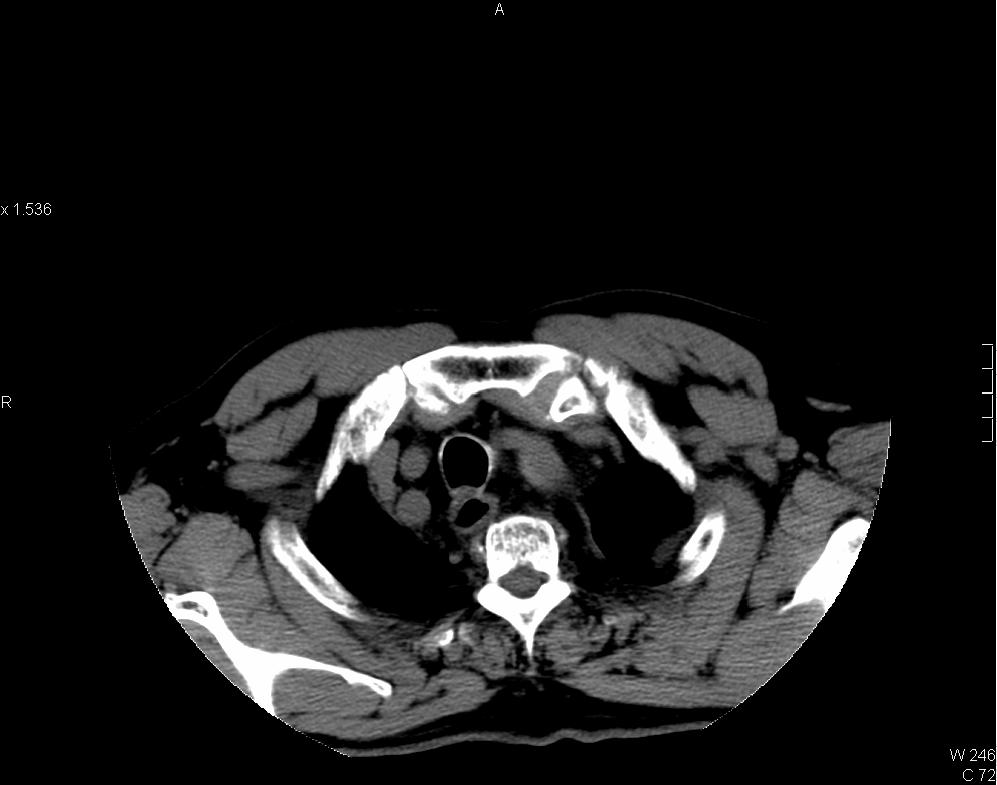
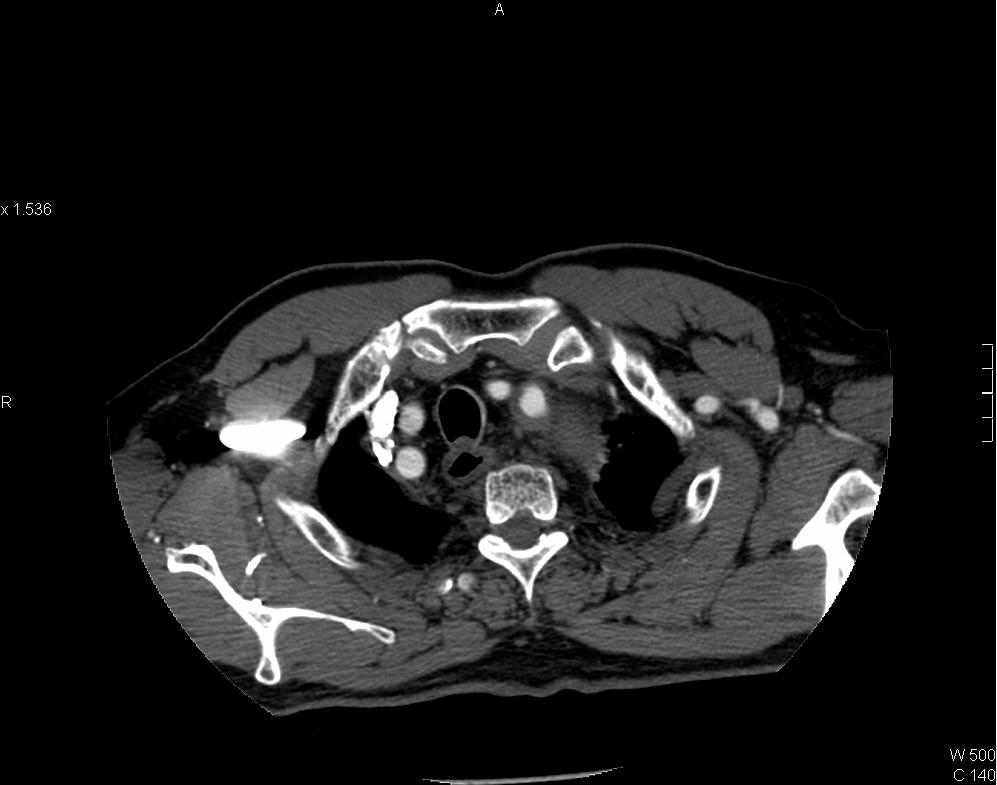
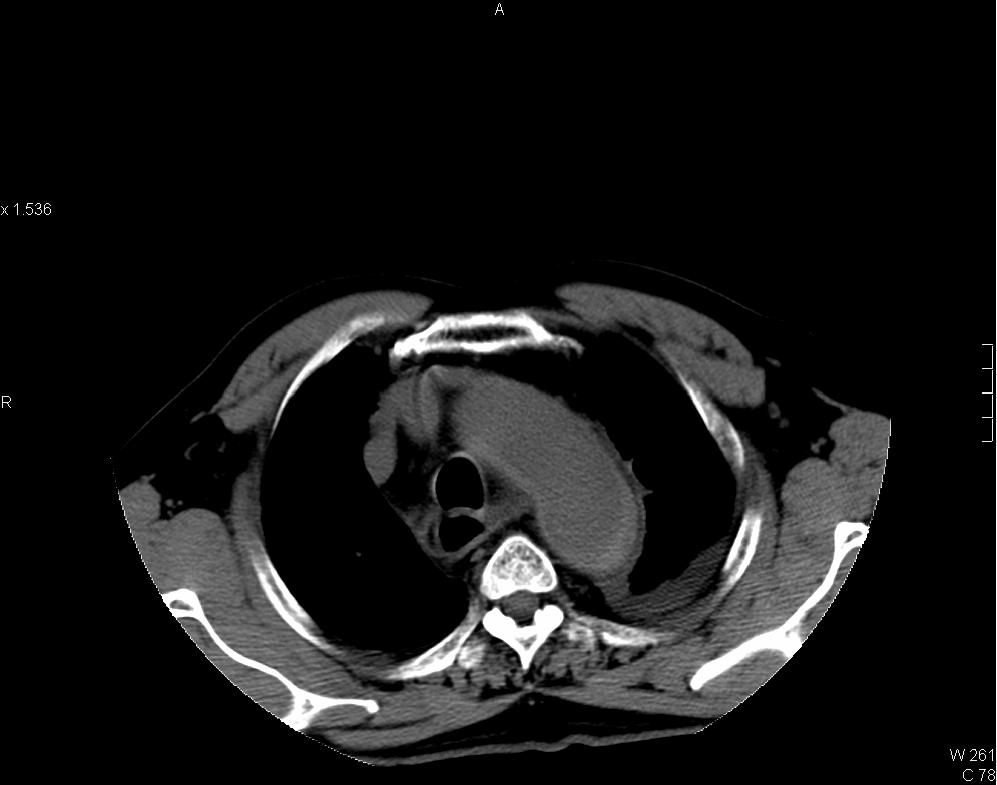
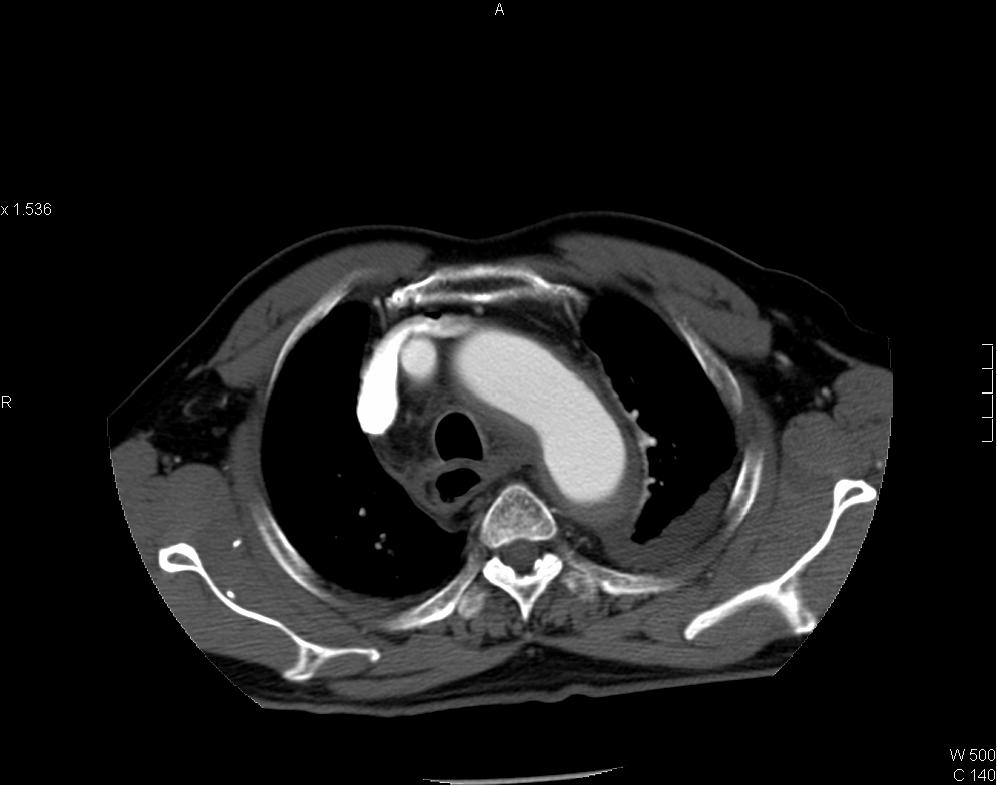
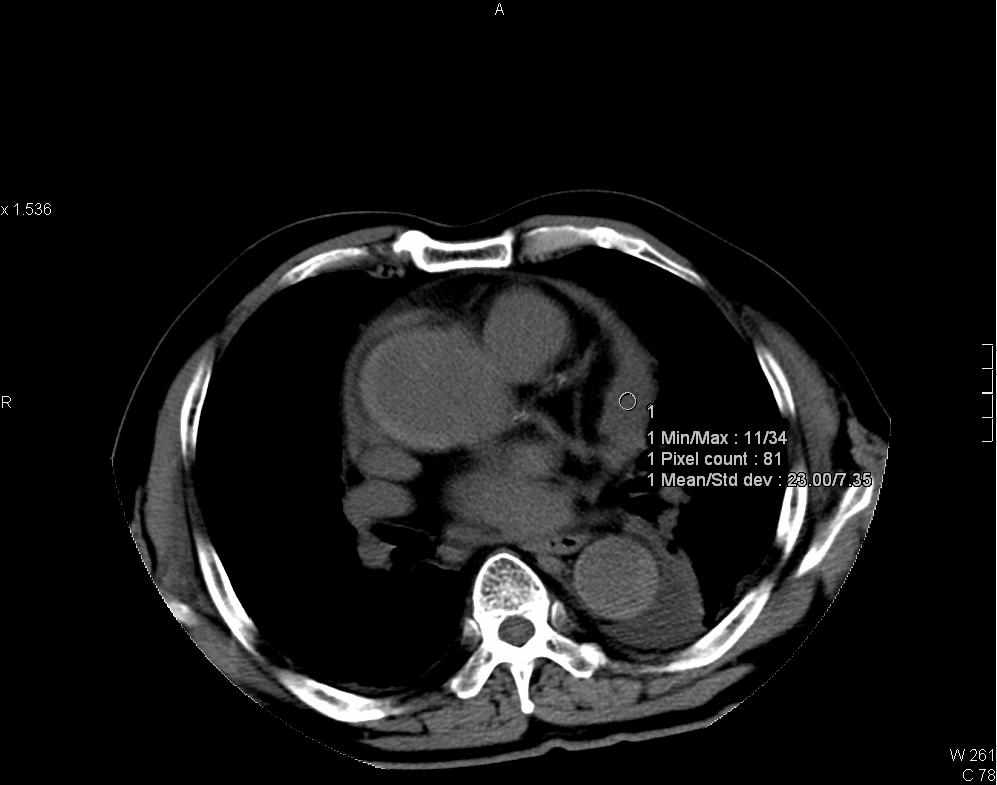
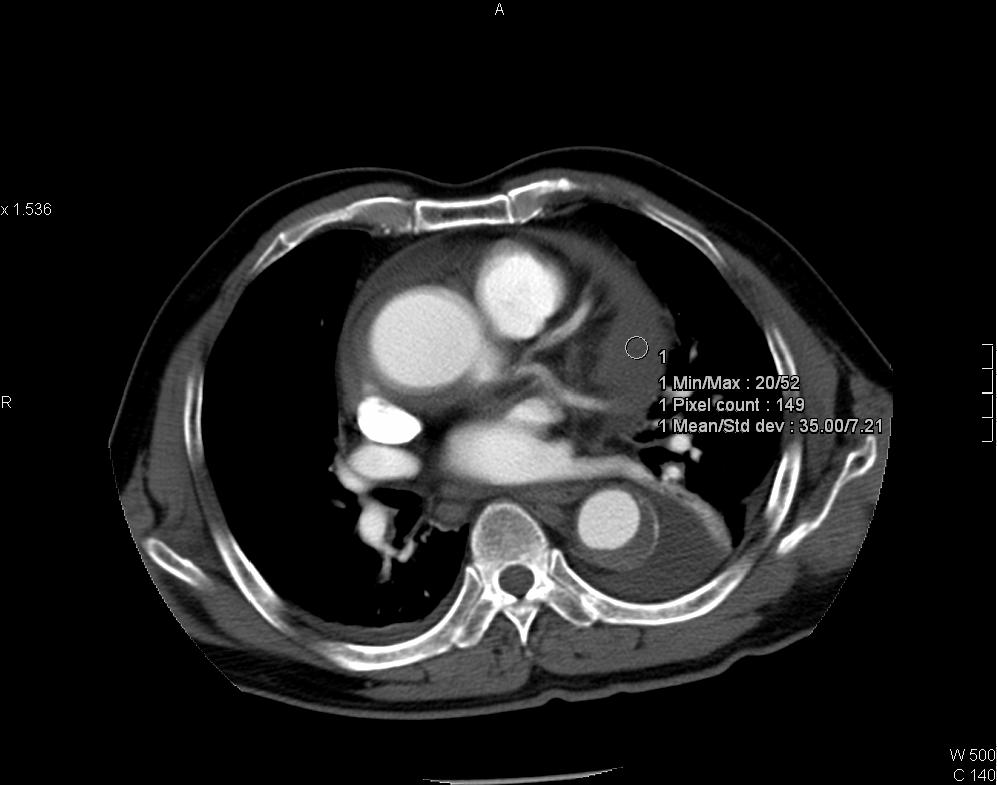
CT thorax showing intramural hematoma (IMH) of aorta in Stanford type A distribution. IMH appears as hyperdense aortic thickening in pre-contrast images and it is relatively hypodense to enhanced luminal blood in post-contrast images. Left subclavian artery is involved. Pericardial collection of intermediate CT number (~35HU) is suspicious of hemopericardium. Resection and replacement of aorta with interposition graft performed and intra-operatively confirmed the presence of hemopericardium.
Intramural hematoma of aorta is caused by spontaneous rupture of aortic wall vasa vasorum. The condition is considered by some authors as an early stage or a variant form of aortic dissection [2]. It shares similar clinical presentation and risk factors with typical aortic dissection such as hypertension, Marfan syndrome, aortic coarctation and cocaine use. CT scan is the investigation of choice. Unenhanced CT shows crescent or circumferential area of aortic hyperdensity, intimal calcifications may be displaced. IMH tends to remain unenhanced in contrast-enhanced CT [1]. Classification and treatment parallels to aortic dissection, those involve ascending aorta and/or aortic arch branches (brachiocephalic, left common carotid and left sublclavian arteries) are considered as Stanford type A IMA whereas those distal to left sublclavian artery are type B IMA.
Basically treatment is surgical for type A IMH whereas aggressive antihypertensive therapy with imaging follow up for type B. Surgery in type B IMH is reserved for those with recurrent chest or back pain despite aggressive therapy, progression to type A disease, aortic dilatation >6cm, ulcer like projection >2cm depth [2].
Complications of IMH include progression to aortic aneurysm, pseudoaneursym and aortic dissection [2]. There are few predictors for progression to overt dissection, include greater thickness of IMH, flattening of aortic lumen, ascending aorta involvement, presence of pericardial or pleural effusion [1, 2].