Answer of May 2008
Clinical History:
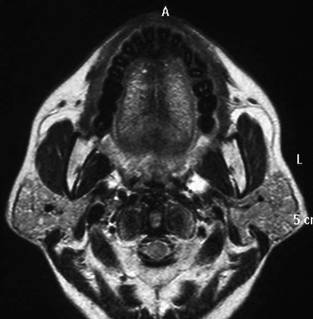
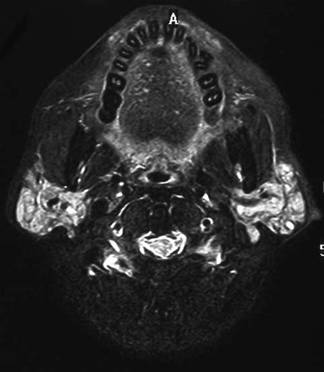
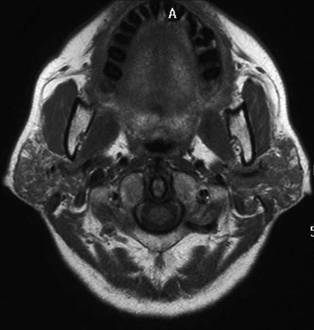
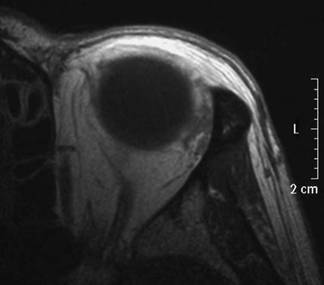
A 42-year-old lady, who previously enjoyed good past health, has been suffering from progressive dry eye and dry mouth for 6 months. She was afebrile all along. Physical examination revealed painless enlargement of both parotid glands. Blood test for autoimmune markers found positive for anti-nuclear antibody. MRI orbit and neck was performed (T2W, T2W FS, T1W images):
Diagnosis:
Sjogren's syndrome
Discussion:
MR orbit and neck shows enlarged parotid and slightly prominent lacrimal glands. Both parotid glands show heterogeneous honeycomblike internal pattern with hyperintense T1W and intermediate T2W signal. Sialectasis is also noted with rather symmetrical involvement. Other salivary glands are normal in appearance (not shown).
Together with the typical clinical presentation and positive autoimmune marker, the overall features are compatible with Sjogren's syndrome.
Sjogren's syndrome is an autoimmune multisystem disease of unknown aetiology.
It can be primary or secondary to other autoimmune diseases such as rheumatoid arthritis, systemic lupus erythematosus or scleroderma. It also has known association with thyroiditis.
The syndrome is characterized by inflammation and destruction of exocrine glands, primarily lacrimal and salivary glands. The other mucous glands in conjunctivae, nasal cavity, pharynx, larynx and airway can also be involved. The affected exocrine glands typically show lymphocytic infiltrate with destruction of glandular tissue +/- ductal dilatation, acinar atrophy and interstitial fibrosis.
It usually occurs in middle age or elderly women, marked by keratoconjunctivitis sicca, xerostomia and enlargement of parotid glands. Definitive diagnosis is made by lower lip biopsy. Treatment for Sjogren's syndrome is mainly symptomatic, though immunosuppressant may be helpful in severe cases associated with vasculitis. Patients with Sjogren's syndrome have increase risk of salivary gland lymphoma in parotid gland, believed to be related to marked lymphocytic infiltration of the parotid.