Answer of November 2008
Clinical History:
A 33 years-old-man presented with 6-months history of low back pain and right lower limb weakness. There was no fever, constitutional symptoms or previous traumatic insult. Physical examination was unremarkable. No lower limb neurology or sphincter disturbance. He had past history of pineal germinoma at the age of 17, and was treated with debulking surgery and RT(cranial and spinal). Currently the disease was in remission.
Plain radiographs and MRI of the lumbar spine were performed.
XR-LS-spine (frontal)
MRI
T1W Sagittal
T2W Fat suppression Sagittal
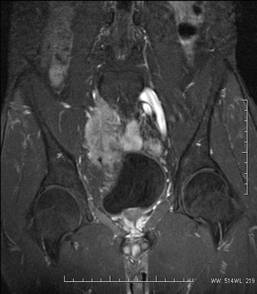
T2W FS Coronal
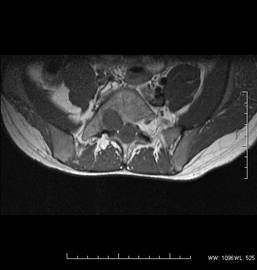
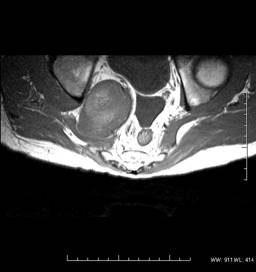
T1W Axial
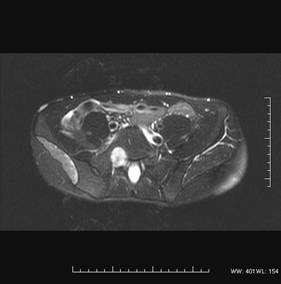
T2W FS Axial
RADIOLOGICAL FINDINGS:
X-ray-
Enlarged right L5/S1 exit neural foramen; Extraspinal soft tissue density superior to right side of urinary bladder (extraspinal portion of the MPNST) in retrospect; VP shunt noted for previous treatment of pineal germinoma complicated with hydrocephalus.
MRI-
T1W Sag: Hypointense lesion exiting via enlarged right L5/S1 neural foramen
T2W fat suppression Sag: Heterogenous hyperintense lesion, with intraspinal extension up to L2-3.
T2W FS coronal: Heterogenous mass (intra- and extraspinal component), the extraspinal portion extends into the pelvic cavity indenting onto the right side of the urinary bladder.
T1W axial: showing widened right L5/S1 neural foramen and sciatic notch
T2W FS axial: showing right gluteal muscle group atrophy secondary to denervation.
Diagnosis:
Malignant peripheral nerve sheath tumor (MPNST)
Discussion:
Peripheral nerve sheath tumors are divided into benign (neurofibroma, schwannoma) and malignant forms (malignant peripheral nerve sheath tumor, MPNST).
MPNST represents 5-10% of soft tissue sarcomas, and usually affects patients in the age range of 20-50. A high proportion (~50%) of MPNST occurs in association with patients with NF-1. On the contrary, only 5% of NF-1 patients would develop MPNST.
There are two forms of MPNST: primary and secondary (related to previous irradiation, with latency period of ~10 years). It is usually the larger major nerve trunks being involved.
Radiologically, there is no absolute reliable criteria in differentiating benign and malignant peripheral nerve sheath tumour.
The following features might raise the suspicion of MPNST,
1. Larger size, >5cm
2. Ill-defined margins, surrounding oedema
3. Heterogenicity with central necrosis (can also seen in benign lesion with degeneration)
4. Calcifications.
5. Site of previous irradiation.
The prognosis of MPNST is dismal. Local recurrence is common. Treatment usually entails a combination of surgery, irradiation and chemotherapy.